#LongCovid is now affecting over 2 million people in the UK, a “mass disabling event” harming health and livelihoods. In the US, where it is reported over 20 million are afflicted with the condition, Long Covid is being described as the “next public health disaster” with an “economic impact rivalling the Great Depression”.
At Attomarker we believe we are approaching potential answers to pressing questions. Antibodies are a key element of our immune systems. Looking at patient antibody responses across a range of Covid variants, it is clear that individual immunity and hence vulnerability varies markedly – we are terming these individual responses immunity endotypes.
Does a particular antibody response to SARS-CoV-2 enable the persistence of micro-colonies of the coronavirus? Viral persistence is thought by many to be a key cause of Long Covid.
We have developed a Multi-Variant Antibody Immunity Spectrum Test, only requiring a fingerprick of blood, that we believe could be used in targeting treatments for Long Covid patients. It is a research test that, unlike our CE marked test, is not yet licensed to be sold to the public and is not available on the NHS, but the good news is that this promising new test and any subsequent treatment can be arranged privately with an appropriate clinician on a named patient basis. The clinician would be interested in your antibody immunity spectrum and seek to identify your endotype. The immunity spectrum could then inform a possible treatment in discussion with your doctor (and keep in mind that some drugs may be expensive).
We have formed a partnership with a clinic specialising in Long Covid (note this is a private clinic). More information is available here: https://recognitionhealth.com/struggling-with-long-covid/
Or email Longcovid@re-cognitionhealth.com to arrange a test.
THE KEY IDEA: LONG COVID PATIENTS HAVE A WEAK IMMUNITY ENDOTYPE RENDERING THEM UNABLE TO CLEAR THE VIRUS COMPLETELY
We hypothesise that a poor immunity endotype leaves one more susceptible to #Covid and #LongCovid. One further hypothesis, which is gaining ground amongst scientists, is that recovery from an infection requires a strongly sterilising serum containing high concentrations of high-quality antibodies. Otherwise microcolonies of the Covid virus (SARS-CoV-2) can circulate anywhere in the body, potentially to the heart or the brain, triggering a T-cell response in the infected cells. This can lead to an inflammatory event and cause repeat sickness, and may increase the risk of developing or extending #LongCovid.
POTENTIAL THERAPIES FOR LONG COVID PATIENTS WITH A WEAK IMMUNITY ENDOTYPE
The Long Covid endotype hypothesis suggests some potential therapies for “plugging the immunity gap”. We have identified certain immunotherapies, sometimes given to reduce the spread of Covid-19 throughout the body, may help to control Long Covid and reduce severe symptom risk – but we have found, with our clinical partners, that the efficacy of these treatments depends on an individual patient’s levels, balance and quality of antibodies. Evidence of clear immunity “dropouts” against particular variants is revealed by our test. The benefit of administering current immunotherapy drugs to those with #LongCovid appears to depend on knowing the precise antibody spectrum, a protocol that we have refined using our unique assay technology, and are putting into practice with our clinical partners.
Phase 2 of the treatment has been developed to “repair the immunity gap” once the sterilising serum has done its work. Encouragingly we have also seen some evidence that a poor immunity endotype may be improved by, for example, switching vaccines – that is, seeking to alter the ‘immunity imprint’. Our recent paper on MedRxiv shows that switching vaccines may change the endotype for some individuals; so a Long Covid patient may benefit from smart-testing, precisely targeted and personalised immunotherapy, then smart-boosting with a different vaccine. Different vaccine combinations may be effective for certain individuals, following on from the results of their antibody immunity spectrum testing and an analysis of their vaccine histories.
A before and after Attomarker immunity profile would be conducted to see to what extent these interventions have worked.
Knowing your immunity endotype should also inform potential levels of protection in light of new emerging variants and assist decision-making around risk for you, your family and society more widely.
If you do not have Long Covid, but are vulnerable due to your health status, knowing your immune response is very important; scientists recommend cancer patients, for example, are tested for antibodies to SARS-CoV-2.* In the event of infection, anti-virals like Paxlovid and Molnupiravir are often only prescribed by Hospital Consultants. Evidence of a weak antibody response may be helpful in the interaction between your personal physician and the consultant when considering your case history.
SUMMARY OF ATTOMARKER RESEARCH AND FURTHER READING
Our new Attomarker multi-variant antibody spectrum research test looks at both concentration of Spike antibodies and their quality (affinity or “stickiness”). We are now measuring these endotypes and producing results consistent with the weak endotype theory. If antibody levels are low and declining, then the sterilising serum will become less and less effective.
The key hypothesis is that personal and precisely targeted immunotherapy enhances the Long Covid patient serum and make it sterilising to clear the virus microcolonies. Furthermore a new vaccine type – a smart boost – may permanently alter your previously weak immunity imprint. If you don’t have Long Covid, and SARS-CoV-2 remains a threat, you might want to know if your variant immunity response is strong across the board. We continue to work on these pressing matters with our hospital and clinical partners.
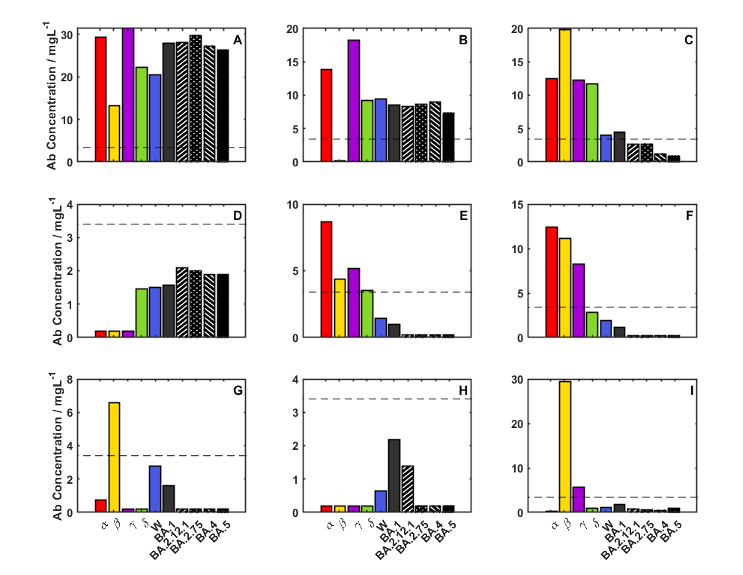
On 11 January, 2023, our Antibody Immunity spectrum study was placed on a pre-pub server – https://www.medrxiv.org/search/attomarker – and shows a full set of immunity endotypes (Figure 1). The ideal antibody response is shown in panel A which is an almost perfect response to any part of the Spike protein that is conserved across all variants – the universal endotype. Looking at panel B however, there is a drop-out endotype for the Beta variant which would suggest that this patient, if exposed to Beta, would mount a poor antibody response and be vulnerable to Long Covid after the infection. More relevant to the current circulating variants are the Omicron dropouts (panels C,E,F,G,H,I) where antibody levels are very poor to the Omicron variants tested, indicating possible vulnerability to Long Covid.
Further reading on recent research: https://www.medrxiv.org/search/attomarker
If you are a clinician and would like to discuss the test with our science team please use this email address: longcovid@attomarker.com
*https://oncology.medicinematters.com/covid-19/vaccines/antibody-testing-sars-cov-2-breakthrough-infections-cancer/23906682 Discussing the results, the team suggests that prevention of SARS-CoV-2 infection “should be prioritized” among those with the lowest level of antibody-derived protection “to minimize impact on their cancer treatments.”
