A Wave Every Three Months
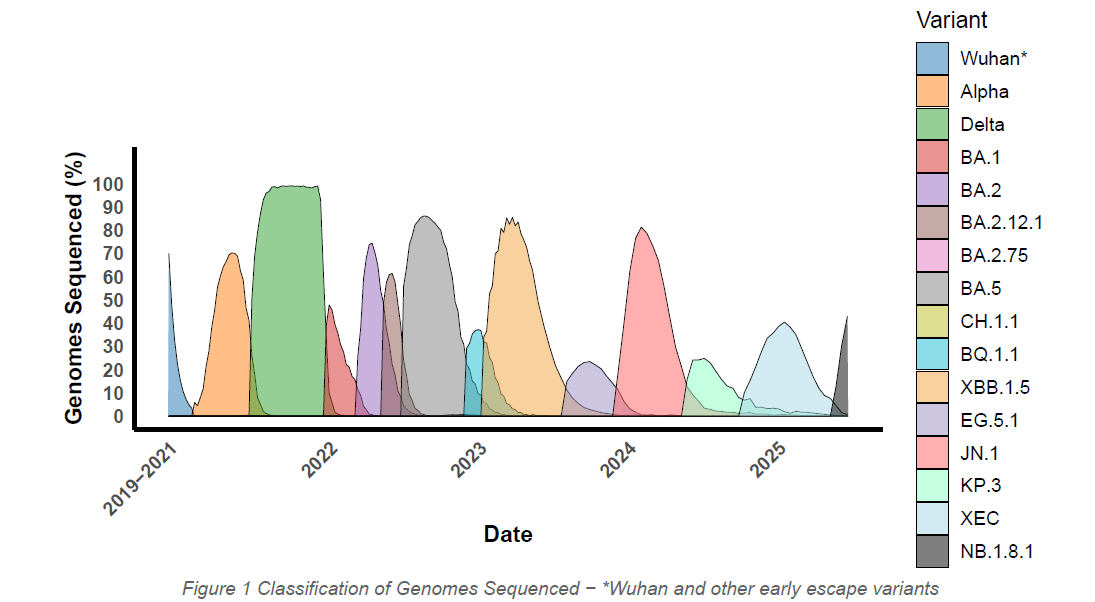
COVID remains with us, with a new variant emerging on average every three months. Nearly 400 million people worldwide are believed to be affected with chronic symptoms such as fatigue, brain fog, and chronic pain; Long COVID. Our research indicates a potential correlation between the waves of COVID variants and gaps in people’s antibody responses to SARS-CoV-2. By comparing the timeline of variant prevalence and the immune profiles generated by our COVID Antibody Spectrum Test, we can begin to understand more about antibody responses, and whether someone has generated a possible hyper- or hypo- immune response to particular variants.
Figure 1 above shows the variant timeline; data collated from the CDC in North America (CDC COVID Data Tracker: Variant Proportions). Data collection began from January 2021, and thus the true prevalence of Wuhan and other early variants is unknown. The values shown for these variants are therefore for illustrative purposes only.
Find your Antibody Classification
Antibody Quantity
Antibody Quality
Why is this important?
The test is not a diagnostic for Long COVID, but our latest research indicates a potential way it can be used to stratify the condition:
- Persistent virus, with identifiable gaps in the antibody spectrum (~65%), indicative of the body being unable to clear the virus. The lingering viral reservoirs in the body are likely to be contributing to triggering symptoms.
- Hyper-immune responses (~10%), where individuals make too many antibodies, and thus overstimulate their immune system.
- The remainder (25%) remain unclassified, and further work is required to fully understand this group.
Understanding personal immune responses opens the door to new treatment strategies, tailored to each person’s unique immune profile. Doctors can use this information to guide targeted treatments, for example, is a monoclonal antibody likely to work? Knowing your antibody concentrations may also reduce the risk of further contraindications from a therapy that is not suited to your immune state.
The test has been used in collaboration with clinical and research partners to profile some interventions such as Evusheld, Sotrovimab, Sipavibart, Pemgarda, and the Novavax vaccine. These are individual case studies at present, and will be written up for peer-review.
The research relating to this work is currently under peer-review; some of the papers are available on a preprint server:
Mass-Standardised Quantitative Measurements of the Antibody Levels for SARS-CoV-2 beyond Correlates of Protection and Clearance medRxiv
James-Pemberton, P. H. et al. Mass-Standardised Quantitative Measurements of the Antibody Levels for SARS-CoV-2 beyond Correlates of Protection and Clearance medRxiv, 2022.2007.2012.22277533 (2025). https://doi.org/10.1101/2022.07.12.22277533
Mass-Standardised Differential Antibody Binding to a Spectrum of SARS-CoV-2 Variant Spike Proteins from Wuhan, Alpha, Beta, Gamma, Delta, Omicron BA.1, BA.4/5, BA.2.75 and BA.2.12.1 variants: Antibody Immunity Endotypes.
James-Pemberton, P. H. et al. Mass-Standardised Differential Antibody Binding to a Spectrum of SARS-CoV-2 Variant Spike Proteins from Wuhan, Alpha, Beta, Gamma, Delta, Omicron BA.1, BA.4/5, BA.2.75 and BA.2.12.1 variants: Antibody Immunity Endotypes. medRxiv, 2022.2009.2023.22280271 (2025). https://doi.org/10.1101/2022.09.23.22280271
Mass-Standardised Antibody Affinity Maturation to the Spike Protein of SARS-CoV-2 Omicron Variants in a Constant-Exposure Cohort: forgiving Original Antigenic Sin.
James-Pemberton, P. H. et al. Mass-Standardised Antibody Affinity Maturation to the Spike Protein of SARS-CoV-2 Omicron Variants in a Constant-Exposure Cohort: forgiving Original Antigenic Sin. medRxiv, 2022.2012.2001.22282932 (2025). https://doi.org/10.1101/2022.12.01.22282932
An Explanation from Prof. Andrew Shaw
This video clip is an excerpt from the first episode of our Prof Talks podcast where Professor Andrew Shaw explains the science behind the Attomarker COVID Antibody Spectrum Test.
View the transcript here
Andrew: Making sure we’re on the same page, the persistent virus idea comes from the fact that you get an acute infection. The virus goes into your body, and it permeates through your lungs and the rest of your body, and while you’re unwell, you get the flu-like symptoms, you get the sickness and the damaged cells into which the virus has entered get repaired by your entire immune response. At the end of that process you’ve got to clear it, and then for a period of time there may be some ongoing symptoms. It takes a while to clear.
And then it leads into the long Covid problems. And it’s probably because there are viral reservoirs and the virus is hanging around your body — in your lungs, in your digestive tract, in your heart, your brain — and causing inflammation, maybe causing autoimmunity, maybe causing gut dysfunction, and that leads on to this 250 symptoms of long Covid.
Why so many? Well, the front door for the virus is this thing called the ACE2 receptor, and it will enter cells wherever they happen to be — whether in your brain, within your lungs, within your liver. All these parts in green have ACE2 receptors, and that’s the problem. It’s difficult to clear from all these regions.
ACE2 is the front door, and this is the bit on the virus that allows it to go through the front door. It’s called its spike protein, and it joins into these ACE2 receptors around the body. So what our test does is measure how well you make these things — these are the antibodies — and it measures how well you make antibodies to the spike protein, not just how many.
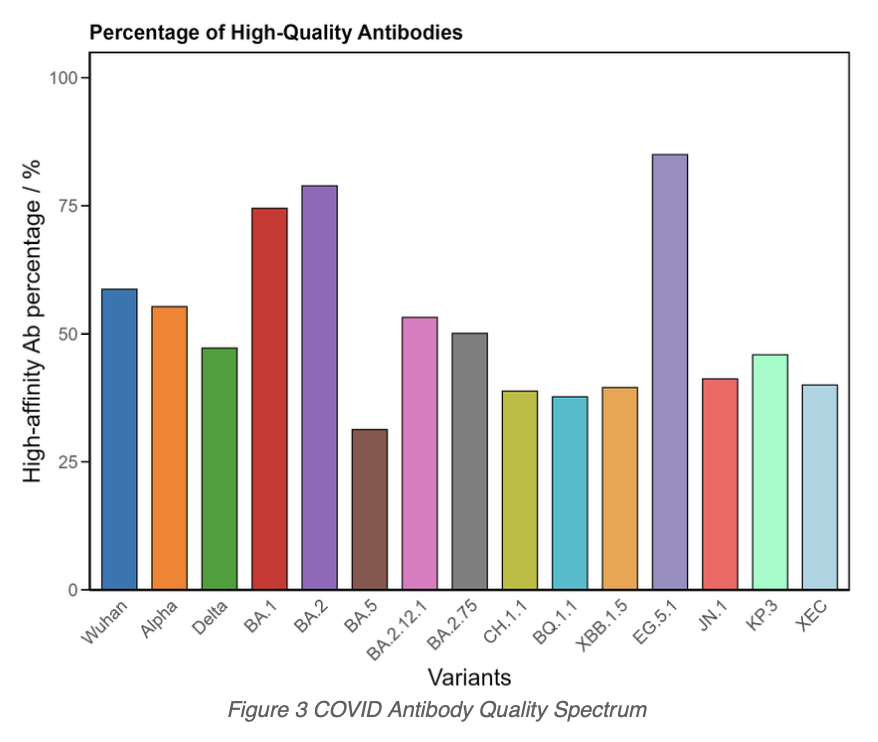
And you do need enough to get all around to all the corners of the body, but also how good they are. What’s the quality of antibody? And that’s our novel part of the test. That’s the bit that makes us different from the rest. The sticky bit is important, because here’s the virus. The antibody sticks to it. If it doesn’t stick for long enough — and long enough is about 2 hours, we’ve just learned — then all these processes here that have the immune system attack the complex and then clear it finally, don’t work. If this drops off, it doesn’t get cleared.
Not only do I have to get the antibodies all around your body — the virus is in your head, it’s in your lungs — I’ve got to get a large concentration everywhere. When they find the virus, it’s got to stick.
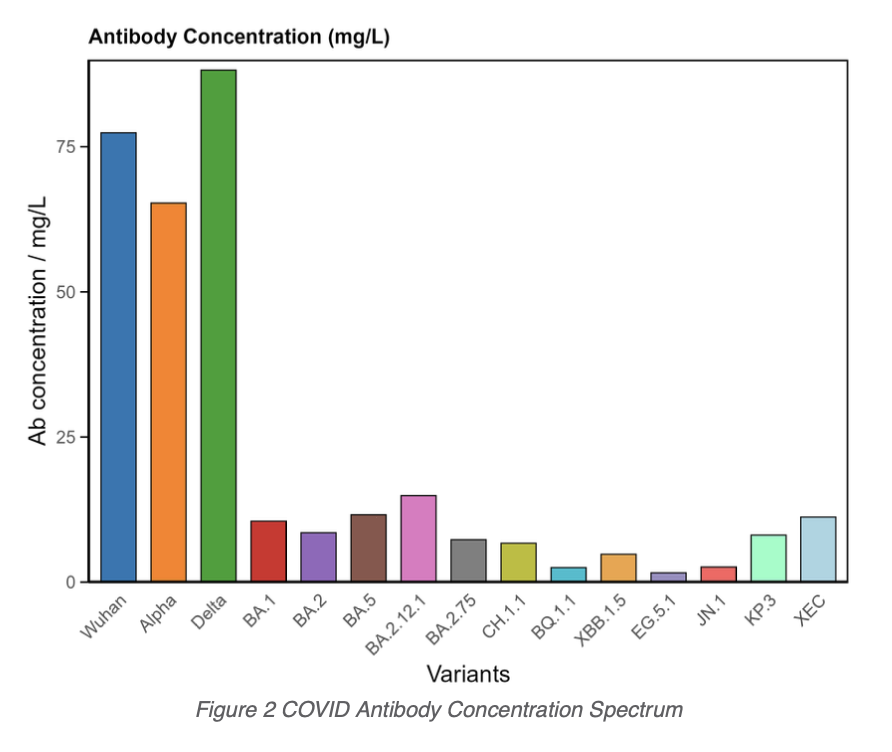
So what we’ve done is to measure the antibody concentration against the spectrum of 14 spike proteins from 14 variants, all the way from Wuhan up to KP.3 at the moment — so two more than I mentioned on this slide.
What you want ideally is you make good antibody concentrations to all variants. And this is a person who’s had a series of vaccines and a couple of infections, but is making good quantity of antibodies to all variants. And this quality is the important number — around 50% or so — means those antibodies stick for a couple of hours.
When we look at the long Covid community, they often have poor antibodies. They didn’t make enough to start with — either from infection or vaccine. Maybe that’s a general problem, maybe they’re always immunocompromised. But they’ve got gaps in their spectrum, usually around quality.
So here’s another long Covid patient here. Quite a good response to the antibodies made from the vaccines — these are the early variants triggered by the vaccines — but none of the later variants are making good quality antibodies. And so if you had an Omicron infection that generated your long Covid, you’re not going to clear that from the body. Nothing sticks around for long enough to help it clear.
This persistent virus therefore accounts for — we’ve learned recently — about 65% of the long Covid community. We’re about to publish this paper, it’s being reviewed by the authors at the moment. We’re going to the journals. And I think this is the big jump. The community divides into groups. 65% have this persistent antibody problem — persistent virus problem.
There’s 10% of the community who have hyperimmunity. They’re making huge concentrations of antibodies. They’re all really good quality. But it’s not clearing the disease somehow. And we’ve seen this at 200 milligrams per liter — this is almost the maximum rate at which you can make antibodies. Why is that being triggered? This hyperimmune, autoimmune response is about 10% of the population. The antibodies don’t go away, and they’re not clearing up the symptoms.
And then I’ve got about 25% of the population for whom my test doesn’t say anything. They may be suffering from other diseases like Lyme disease or resurgent Lyme disease, but for the moment I can’t tell the difference.
So what are the treatment options? If you get your spectrum measured and we find the gaps and they align with your clinical history, you can plug the gaps. For that 65% of people that have got bad antibody spectra, with Sotrovimab, Evusheld — with the antibodies available at the beginning of the pandemic. But Cipavibart is the one that’s out there at the moment, made by AstraZeneca, and we’re trying to get hold of this in the UK. We’re chatting frequently to AstraZeneca about getting it. It is available in Europe; it’s not yet available in America.
The other option we tried is vaccine. This is a protein vaccine, not a messenger RNA vaccine, and it is made by Novavax and Sanofi. They had it out for a while. We tried it in a few patients — and I’ll show you those results in a minute — but it’s now no longer available.
But it doesn’t mean that 35%, the hyperimmune and the unclassified group, need to go to the doctor now. Because the hyperimmunity will give the doctor some idea about what to do. The unclassified might be because it’s Lyme disease, it might be because it’s Epstein-Barr virus, and the doctors with whom we’re collaborating — people like Dr. Ben Sinclair, Dr. Finlayson, and Dr. Binita Kane — they’re coming up with tailored responses to those options. So there may be ways to manage these, even if I don’t know yet as a scientist what’s causing them.
So this is what the Evusheld did. Here’s a patient here — reasonable antibodies, but a gap in their quality. We gave them Evusheld. We gave much higher concentration of antibodies that trebled the antibody concentration — good quality antibodies.
This patient was bedbound in their bedroom, not awake for very long during the day, migraine every day. By the end of the first jab, their gut function improved significantly, their migraine frequency had dropped to one a month, and they started getting better.
And we started measuring. Here’s the concentration rising over time. And after the third jab, they felt so much better they ruined my graph and went to Greece on holiday. So it looks like this intervention for this patient worked well.
And the bit that’s really interesting — this is very rarely seen in science — this is the antibody spectrum in their blood, but this is the antibody spectrum in their cerebrospinal fluid. This is the whiskey-like liquid around your brain. That shows that the antibody was getting into your brain. That shows we were putting enough antibody in their blood to get to the point where things like the brain fog could be treated. So that’s a really exciting result. We need to do that more often.
We’ve done antibody interventions on two people, and there are lots of people interested in getting antibody interventions if we can get it into the UK — or get the patient to Europe.
Novavax — we’ve tried. So here’s an antibody spectrum of a patient, long Covid patient, gaps in their spectrum for quality. After one jab of vaccine, we repaired that spectrum. They started getting better. They had three jabs to make sure these levels got higher, and they’re showing an onward trajectory in the improvement of their symptoms.
So that’s quite encouraging.
This patient, however, is hyperimmune. This antibody level doesn’t change very much, and she was going to hospital once a month or so with complications around her condition.
Once the doctor saw it was autoimmune — potentially autoimmune — interventions around steroids to reduce inflammation and other drugs to suppress the autoimmune response were considered. And her position is now being managed really carefully.
Viv is very excited about the fact that first of all, we showed that there was a problem — and before, people just weren’t believing her — but also after that it got managed properly.
So that’s what the Atomarker test is showing. And these treatment options for people. And that triggers all the questions, Jonathan. So I think we should try.
Jonathan: Lot to unpack there, Andrew, thank you very much.

Trusted by Clinicians
“We need to investigate the causes and treatment of viral persistence. We have been using the Attomarker test to identify our patients with persistent COVID activity.”
Dr Ben Sinclair
Long COVID Specialist
featured in The Sunday Times

Trusted by Patients
“Attomarker’s blood test has been a game changer, enabling me to understand and manage my Long COVID. There’s nothing else like it available through NHS Long COVID clinics.”
Patient Testimonial